Gum disease affects millions of people worldwide and poses significant risks to both oral and overall health. Ranging from mild conditions like gingivitis to more severe forms such as periodontitis, these infections can lead to tooth loss and are linked to broader health issues if left untreated.
This article delves into the most common forms of gum diseases with insights into their symptoms, causes, and effective treatment strategies. Whether you’re experiencing early signs of gum discomfort or seeking preventive measures, our comprehensive guide aims to empower readers with knowledge and practical advice to maintain optimal gum health and safeguard their smiles.
What Is Gum Disease?
Also known as periodontal disease, gum disease is an infection of the tissues that hold your teeth in place. It’s typically caused by poor brushing and flossing habits that allow plaque—a sticky film of bacteria—to build up on the teeth and harden. In advanced stages, gum disease can lead to sore, bleeding gums, painful chewing problems, and even tooth loss.
What Are the Different Types of Gum Disease?
Gum disease can appear as gingivitis or periodontitis, each representing different stages of severity. Gingivitis, the initial stage, involves gum inflammation without affecting the bone, while periodontitis, a more advanced condition, can lead to significant damage to the soft tissue and bone that support the teeth. Understanding these types is crucial for effective treatment and maintaining overall oral health.
 Gingivitis
Gingivitis
Gingivitis is the earliest and mildest form of gum disease, characterized by red, swollen, and bleeding gums caused by plaque buildup at the gum line. If treated promptly, gingivitis can be reversed with professional dental care and improved oral hygiene, preventing progression to more serious gum diseases.
Periodontitis
When gingivitis is left untreated, it can advance to periodontitis, where the inner layer of the gum and bone pull away from the teeth and form pockets. These small spaces between teeth and gums collect debris and can become infected, leading to bone loss and the loss of connective tissue that holds teeth in place.
Advanced Periodontitis
In this final stage of gum disease, the fibers and bone supporting your teeth are destroyed, causing your teeth to shift or loosen. This can affect your bite and, if aggressive treatment isn’t sought, may lead to tooth extraction to prevent the spread of infection.
Chronic Periodontitis
Chronic periodontitis is the most common form of periodontitis, mostly affecting adults but can occur at any age. It involves the slow deterioration of the supporting tissues of the teeth, with periods of rapid progression. Consistent treatment and maintenance from a Plantation dentist can help manage the condition and prevent tooth loss.
Necrotizing Periodontitis Disease
This severe form of gum disease occurs when the infection leads to the necrosis (death) of gingival tissues, periodontal ligaments, and alveolar bone. It’s most commonly seen in individuals with systemic conditions such as HIV, immunosuppression, or malnutrition, requiring immediate medical and dental intervention.
What Are Early Signs of Gum Disease?
Recognizing the symptoms of gum disease is crucial for early intervention and treatment. Common signs include persistent bad breath, red or swollen gums, bleeding during brushing or flossing, receding gum lines, and loose or shifting teeth. Identifying these symptoms early can significantly improve the effectiveness of treatment and prevent the progression of gum disease to more severe stages. If you have any of these symptoms, it’s best to schedule an appointment with a dentist in Plantation, Florida to ensure timely and appropriate care.
Bleeding Gums
One of the earliest signs of gum disease is gums that bleed easily during brushing or flossing. This symptom indicates inflammation caused by plaque accumulation at the gum line and should not be ignored, as it’s a clear sign that your gums require attention.
Receding Gums
Gum recession occurs when the margin of the gum tissue surrounding the teeth wears away or pulls back, exposing more of the tooth or the tooth’s root. This can lead to sensitivity and is often a result of advanced gum disease.
Swollen or Tender Gums
Healthy gums are firm and pink. If your gums are swollen, red, or tender, it could be a sign of gum disease. This inflammation is a response to the toxins produced by plaque bacteria attacking the gums, signaling the need for improved oral hygiene or professional treatment.
Chronic Bad Breath
Persistent bad breath or a bad taste in the mouth that doesn’t go away with brushing or flossing can be a symptom of gum disease. The bacteria causing the disease produce foul-smelling waste products, contributing to this uncomfortable condition.
Loose or Shifting Teeth
Advanced gum disease can lead to the deterioration of the supporting bone and tissues, causing teeth to become loose or shift in position. This can affect your bite and, if untreated, may lead to tooth loss. As a result, it’s essential to address gum disease promptly to prevent these severe outcomes and preserve your oral health.
What Are the Leading Causes of Gum Disease?
The leading causes of gum disease stem from a combination of factors that contribute to the buildup of plaque. Poor oral hygiene is the primary culprit, as it allows plaque to harden into tartar, which is much more difficult to remove and irritates gum tissues. Smoking significantly increases the risk and severity of gum disease, as it impairs the body’s ability to heal tissues, including those in the mouth.
Additionally, hormonal changes, such as those during pregnancy, puberty, and menopause, can make gums more sensitive and susceptible to gum disease. Underlying conditions like diabetes and certain medications can also affect gum health.
Poor Oral Hygiene
Poor oral hygiene is a major cause of gum disease. Neglecting regular brushing and flossing allows plaque to accumulate on teeth and along the gum line, leading to inflammation and infection. Over time, tarter left on the teeth can advance the progression of gum disease if left untreated.
Smoking or Chewing Tobacco
Smoking or chewing tobacco significantly increases the risk of developing gum disease. Tobacco use impairs blood flow to the gums, hindering the body’s natural healing processes and making the gums more susceptible to infections. Additionally, tobacco can contribute to the buildup of plaque and tartar, advancing gum inflammation and disease.
Genetics
Some individuals are genetically predisposed to gum disease, with family history playing a crucial role in their oral health. This genetic factor can influence susceptibility to infections, including those affecting the gums, making some people more prone to developing periodontal issues despite maintaining good oral hygiene.
Hormonal Changes
Hormonal changes, particularly in women during puberty, pregnancy, menopause, or menstrual cycles, can make gums more sensitive and vulnerable to gum disease. These changes can affect the blood flow to the gum tissue, increasing the risk of inflammation and infections.
Diabetes
People with diabetes have a higher risk of gum disease due to their greater susceptibility to infections. Poor blood sugar management can lead to more serious forms of gum disease since diabetes affects how the body processes blood sugar, endangering the health of gums and other bodily tissues.
Autoimmune Diseases
Autoimmune diseases, where the body’s immune system attacks healthy cells, can contribute to gum disease. Conditions like rheumatoid arthritis and lupus can lead to inflammation throughout the body, including the gums, making gum disease more likely and potentially more severe.
Nutritional Deficiencies
A lack of essential nutrients, particularly vitamins A and C, can impair the health and healing capacity of gum tissue. Nutritional deficiencies weaken the body’s defense against infections, including those that lead to gum disease, by affecting the integrity and resilience of the gums and oral tissues.
Common Gum Disease Treatments
Treating gum disease effectively requires a tailored approach based on the severity and progression of the condition. From non-invasive methods like professional teeth cleaning to more advanced treatments such as scaling and root planing or surgical interventions, the goal is to halt the disease’s progress, restore gum health, and prevent tooth loss. There are many treatments available for gum disease, however, the importance of early detection and personalized care is the best way to reduce potentially serious oral health issues.
Professional Teeth Cleanings
Regular professional cleanings are crucial for removing plaque and tartar buildup that brushing and flossing at home can’t eliminate. In-office teeth cleanings help prevent the progression of gum disease by keeping the gum line and spaces between teeth clean and free from harmful bacteria.
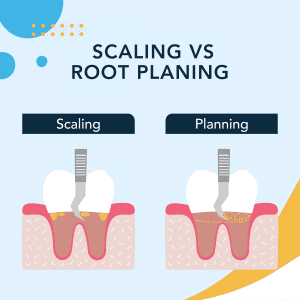
Scaling & Root Planing
This deep-cleaning procedure involves removing plaque and tartar from above and below the gum line (scaling) and smoothing rough spots on the tooth root (planing). Scaling and root planing help gums reattach to teeth and reduce periodontal pocket depths.
Antibiotics
Antibiotics can be used to fight gum infections. They may be prescribed as a mouth rinse or as a gel applied directly in the gum pockets after scaling and root planing, helping to reduce bacteria and inflammation associated with gum disease.
Gum Graft Surgery
For advanced gum recession, gum graft surgery involves taking tissue from another part of the mouth (often the palate) and attaching it to the affected area. This procedure covers exposed roots, reduces further recession, and improves the aesthetics of the gumline.
Flap Surgery
Also known as pocket reduction surgery, flap surgery involves lifting back the gums to remove tartar deposits in deep pockets. The gums are then sutured back in place to fit snugly around the tooth, reducing the space for bacteria to grow.
Bone Grafting
In cases where gum disease has destroyed the bone supporting your teeth, bone grafting can help regenerate lost bone and tissue. Materials that encourage your body’s natural bone regeneration are placed in the affected areas to provide stability for teeth.
Guided Tissue Regeneration
Guided tissue regeneration is a procedure that encourages the regrowth of bone and tissue lost to gum disease. After removing bacteria, a small piece of biocompatible fabric is placed between the bone and tooth, preventing unwanted tissue from entering the healing area and allowing bone to grow back.
Laser Treatments
Laser treatments involve using high-intensity light to remove diseased gum tissue and kill bacteria without the need for scaling and planning. This method reduces bleeding, swelling, and discomfort and may promote faster healing and tissue regeneration compared to traditional surgery.
Schedule a Dental Checkup in Plantation, FL
If you’re concerned about gum disease or other oral health issues, scheduling a dental checkup is a proactive step towards maintaining good oral health. It is important to find a dentist near me that is equipped with the latest technology to diagnose, treat, and prevent oral health problems. By scheduling an appointment with a trusted Plantation dentist, you’ll receive personalized care that is tailored to your specific needs to ensure your smile remains healthy and bright. Don’t wait for gum disease symptoms to worsen; prioritize your oral health today.
February 16, 2024

 Adult
Adult